How Cube Therapy Billing Cut ABA Denials Below 5% and AR to 21 Days
- Veronica Cruz

- Sep 9, 2025
- 4 min read
Updated: Sep 10, 2025
A behavioral health group wanted to expand across states but hit billing and credentialing roadblocks. Their RCM process was messy: claims sat in AR for months, denials piled up, credentialing was delayed, and payors weren’t being challenged on incorrect EOBs.
Here’s what was happening:
Breakdowns in communication between providers and the billing team.
High credentialing denials because applications weren’t tracked or updated in CAQH.
Aged AR was growing because claims weren’t followed up on systematically.
Incorrect denials from major payors weren’t being appealed in time.
No denial tracking or payer trend analysis, which meant repeating the same mistakes.
Lack of clean claim checks before submission, leading to preventable rejections.
The result? Delayed cash flow, frustrated providers, and lost revenue.
Step 1: ABA Billing Audit to Identify Revenue Leakage
We started our ABA billing audit with a denial analysis and reviewed AR buckets (30–60, 60–90, 90+ days).
Looked at CPT code usage and modifiers.
Checked timely filing compliance.
Reviewed payer EOBs to identify recurring denial codes.
Audited credentialing files and CAQH attestations.
This gave us a clear map of where revenue leakage was happening.
Step 2: Clean Claim Process in ABA Therapy Billing Services
Cube implemented a clean claims protocol before submission:
Claims were scrubbed for missing modifiers, POS (place of service) codes, and documentation gaps.
Eligibility and benefits were verified before scheduling sessions.
Authorization units and end dates were tied directly to the billing workflow.
This cut down on front-end rejections significantly.
Step 3: Streamlining ABA Credentialing Services
Credentialing denials were eating into revenue. Cube’s credentialing specialists:
Updated CAQH profiles and ensured attestations were current.
Corrected NPI, taxonomy, and address mismatches.
Prioritized payers by reimbursement volume.
Sent weekly credentialing status reports so providers knew where each application stood.
This reduced credentialing turnaround time and brought new providers in-network faster.
Step 4: Denial Management in ABA Billing Services
Denials were the biggest pain point. Cube created a Denial Response Team with strict timelines:
Every denial was reviewed within 48 hours of the EOB posting.
Correctable errors (missing modifier, incorrect CPT code) were reprocessed within 24 hours.
Incorrect payer denials (like bundling or misapplied policies) were appealed immediately with clinical notes and coding references.
Built payer-specific appeal templates to speed up resubmissions.
Step 5: AR Follow-Up in ABA Therapy Billing Services
Aged claims were draining revenue. Cube’s AR specialists:
Called payors on all claims in 61–90 and 90+ buckets.
Logged payer call notes directly into the AR dashboard (no more scattered spreadsheets).
Set reminders for reprocessing timelines.
Escalated chronic delays to payer reps with claim ID lists and documentation.
Step 6: Authorization and Benefits Tracking in ABA Billing Services
Auth denials were a recurring problem. Cube fixed this by:
Standardizing VOB (Verification of Benefits) forms.
Entering the auth start and end dates in the scheduling system.
Creating alerts when units drop below 10% remaining.
Training admin staff to renew authorizations early, preventing gaps in coverage.
Step 7: Coding and Documentation Support in ABA Therapy Billing
Cube’s coding team ran checks on:
CPT 97153, 97155, 97156, and modifiers.
Time-based documentation for direct therapy.
POS codes (telehealth vs in-clinic).
Consistency between session notes and billed time.
By tightening documentation, medical necessity was easier to prove in appeals.
Step 8: Reporting and Dashboards for ABA Billing Services
Instead of waiting for end-of-month surprises, Cube provided:
Weekly denial trend reports by payer.
AR aging dashboards showing which claims were pending and who owned them.
Credentialing trackers are updated in real time.
Monthly scorecards with denial %, reimbursement %, and AR days.
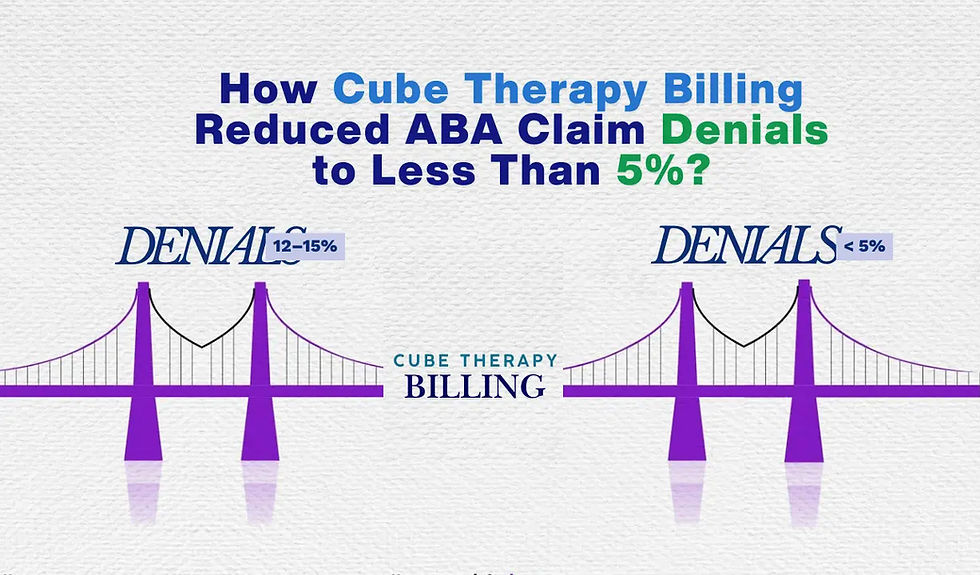
Results Achieved with ABA Therapy Billing Services
The numbers tell the story:
Denial rate dropped below 5%.
Reimbursement improved to 98% of billed charges.
Days in AR dropped to ~21 days, well below the industry average of 45–50.
Timely filing losses shrank because every claim had a follow-up clock.
Providers finally had visibility on credentialing, payer behavior, and AR status.
Why Cube’s ABA Billing Services Delivered Results
Clean claims first. Scrubbing cut rejections at the front end.
48-hour denial response. No denial aged past two business days.
Proactive credentialing. CAQH and payer updates stayed current.
Tight AR follow-up. Daily payer calls and documentation logs replaced “follow-up when possible.”
Data transparency. Dashboards turned billing into a measurable process, not guesswork.
Day-to-Day Improvements with ABA Billing Services
Admin staff saw auth alerts before units ran out.
Providers didn’t have to resend the same paperwork twice.
Billing teams worked out of one queue instead of endless email chains.
Leadership checked live dashboards instead of waiting for reports.
Most importantly, cash flow stabilized and supported expansion.
FAQs
1. Can Cube really maintain denial rates below 5% long-term?
Yes. With eligibility verification, clean claim scrubs, and a 48-hour denial response, denials can stay consistently low. The key is prevention plus quick reprocessing when denials happen.
2. What about credentialing delays when adding new providers?
Credentialing issues often come from incomplete CAQH or payer-specific mismatches. Cube uses a credentialing pipeline that tracks each provider, payer, and status. Weekly updates keep applications moving until approval.
3. What’s the fastest way to improve AR days in ABA therapy billing?
Focus on aged AR (90+ days) with daily payer calls, logged notes, and escalation when needed. At the same time, enforce timely submission so new claims don’t age in the first place. Cube’s process brought AR down to ~21 days, compared to the 45–50 day average.



